5 min
June 1, 2025

5 min
June 1, 2025

Heel spurs, like many other musculoskeletal issues, are a common cause of pain and discomfort, especially among those who lead an active lifestyle or spend long hours on their feet. This condition occurs when a bony growth develops on the underside of the heel bone, often as a result of repeated stress, pressure, or inflammation of the tissues that support the foot.
A heel spur or bone spur is a bony growth that pokes out from the bottom of your heel, where your heel bone connects to the ligament running between your heel and the ball of your foot (the plantar fascia). Heel spurs affect about 15% of people.
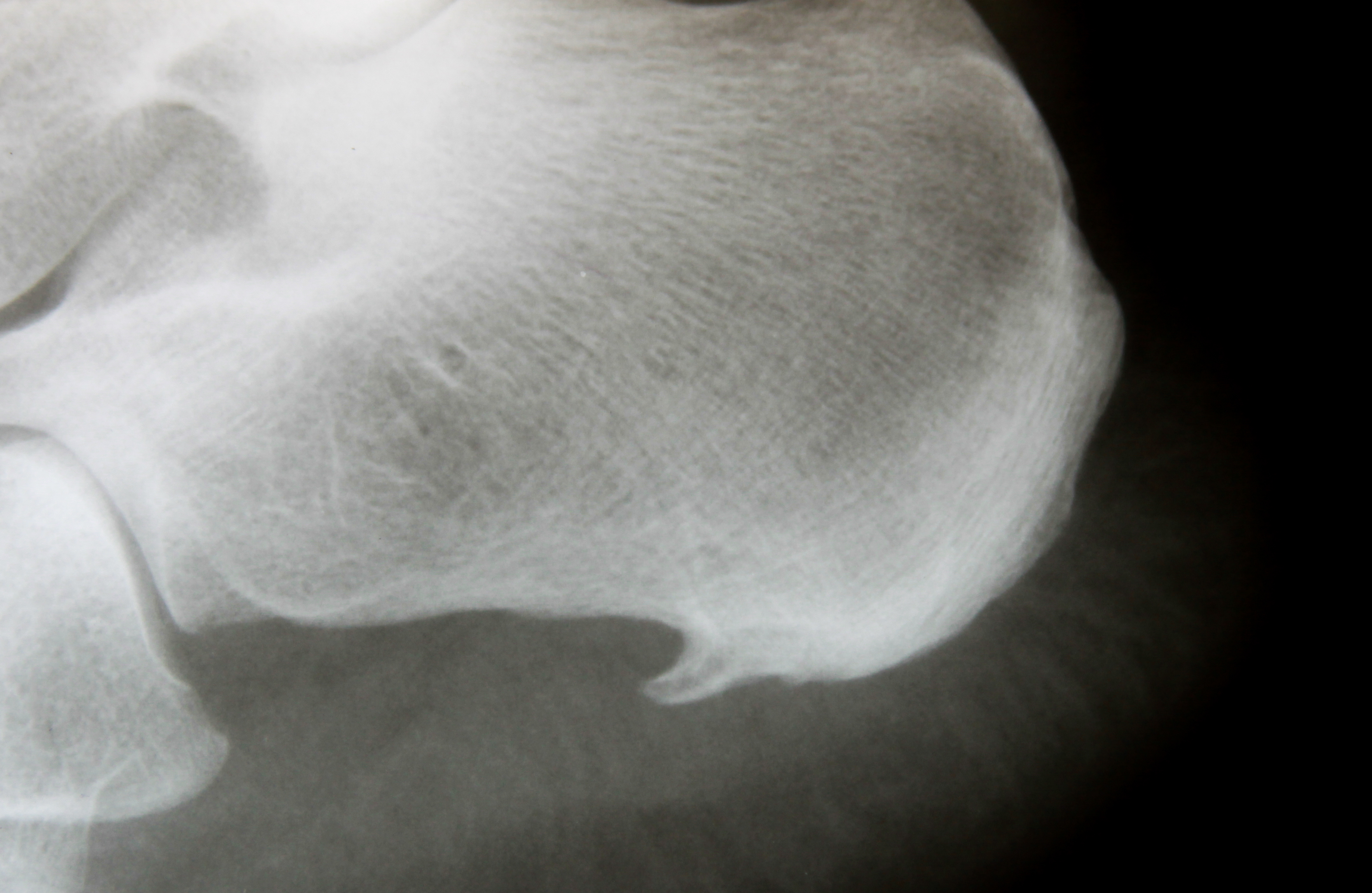
Heel spurs have been shown to develop in response to damage and strain to the soft tissues that insert at the bottom of the heel - in this case, the insertional fibres of the plantar fascia tissue. When the plantar fascia, which connects to the bottom of the heel bone, repetitively pulls on and places stress on the heel during movement, this creates micro-trauma. The body responds by trying to repair the area by creating more bone - this becomes the calcified protrusions that we know as heel spurs.
Anything that exacerbates the pulling and stress on the heel bone from the plantar fascia will contribute to the development of a heel spur, including:
Heel spurs may also be caused by inflammatory arthritis, and may be encouraged by other problems like the breakdown of the fat pad of the heel.
When heel spurs are symptomatic, they can aggravate the tissue that they’re associated with, which in this case is the plantar fascia, producing symptoms including:
Regardless of the annoying pain and tension in the foot, starting the treatment process is often delayed because we simply associate the pain with foot fatigue. However, over time, the pain in the sole increases during rest. So-called initial pain is observed at the beginning of movement, after rest or in the morning, after waking up.
Pain can appear suddenly or gradually increase. Pain is often felt immediately upon weight bearing. The patient feels as if something sharp had pierced the heel. If the pain becomes chronic and a heel spur appears, the person tries to walk on their toes or place their foot on the outside of the heel, not on the heel.

It is very common for our podiatrists to hear that when a person develops heel pain, they quickly suspect that their pain is caused by a heel spur. While ‘heel spurs’ have become a common term to explain heel pain, this isn’t technically accurate, and for over 95% of the patients we see with pain at the bottom of their heel, the true cause of pain is actually a condition called plantar fasciitis.
Heel spurs and plantar fasciitis are related conditions but they're not the same. Here’s how the two conditions intersect:
Due to the similarity in symptoms between a heel spur and other causes of heel pain like plantar fasciitis, confidently diagnosing a heel spur specifically includes taking your medical and injury history, a comprehensive clinical exam, and an x-ray.
Treating a spur at the bottom of your heel follows the same treatment plan as plantar fasciitis, because of the unique way in which the two are connected. This may include:

For almost all of our patients that have heel spurs confirmed with an x-ray, following our proven treatment methods completely resolves all of the painful symptoms, meaning that the heel spur will not require direct treatment with surgery or other methods. If conservative treatment methods fail, however, surgery may be considered as a last resort.
Heel spurs do not go away on their own, as they are bony protrusions from a bone. With this being said, you can make a full recovery from your heel pain even with a heel spur present, so the goal of treatment is not actually to make the spur ‘go away’, as it is to treat your symptoms.
Pain in this disease is simply a defensive reaction of the body. In this way, the body "calls" on the person to protect damaged tissues from further degradation and to provide time for new cells to appear in the disease site.
Taking painkillers (in the form of injections, i.e. blockades, phonophoresis or electrophoresis), using radiotherapy (X-ray therapy), when the nerve receptors signaling pain are blocked, leads to rapid improvement. As a result, the patient feels cured of the disease. However, the consequence of such actions is further development of the disease. As soon as the effects of pharmacological agents or radiotherapy cease, the symptoms return.
Like any other part of the body, the calcaneal fascia is made up of cells. Damage to the fascia means the death of individual cells. Dead cells are shed naturally, thanks to the body's defense reactions. However, this process can be too slow due to the appearance of more dead cells. Due to the constant presence of harmful factors, new injuries occur all the time (after all, you can't suddenly stop walking completely).
Pain occurs when too many dead cells accumulate and the body starts regenerative (inflammatory) processes. Intra-tissue pressure increases in the soft tissue around the heel spur. The idea is to increase the supply of immune cells and ensure their rapid transport through the tissues. The more cells have died, the stronger the reaction and pain.
In practice, anti-inflammatory drugs (especially hormonal ones) are used in the treatment of heel spurs, which are designed to inhibit the defense reactions. The drug works in such a way that the body inhibits its actions of cleansing the tissues in the heel area. As a result, the inflammation goes away and the person feels better. However, the accumulation of dead cells from which the heel spur is formed remains. As a result, the disease may relapse, because sooner or later the effect of the drug will wear off, the body will "wake up" and start the inflammatory process again. This method is dangerous because introducing hormonal drugs into the body often leads to necrosis (death) of the heel bone.
Therefore, a sensible treatment should consist of helping the body to remove dead cells to prevent the formation of a spur. Preference should be given to methods that promote increased microcirculation in the tissues, increased blood and lymph flow (e.g. low-intensity vibration therapy at home, shock wave therapy in an outpatient setting). The inflammatory process will eventually subside if simultaneous actions are taken to reduce the load on the aponeurosis.
Considering the above, effective treatment for heel spurs includes the following steps:
There are currently many methods of treating heel spurs. However, their effectiveness, cost and availability vary. Unfortunately, most of them do not meet all three conditions of effective heel spur treatment. Most methods only work on the heel area and are intended to only reduce or eliminate pain in that area, eliminate swelling and remove the bony growth. As a result, the disease often recurs after some time after the treatment.
However, there is a solution that works not only to reduce symptoms, but also treat the condition. The energy of biological microvibrations can be delivered from the outside using vibroacoustic therapy, known as phonation.
Phonation is the transmission of sound microvibrations (in the frequency range of 30-20,000 Hz) to the body of a person or animal using a special compact medical device. Such sound microvibrations are natural for the body, their physical properties resemble biological microvibrations that appear in muscle tissue during maximum static load.
Fonovit is the device used to accelerate the healing of heel spurs and prevent the deterioration of the aponeurosis. The biophysical effects achieved through the use of the Fonovit device allow for the elimination of the problem within 2-3 weeks. It is common knowledge that all immunological and regenerative processes require the transport of substances and cells to the interaction zone. This is a rather energy-intensive biophysical process, requiring energy derived from mechanical microvibrations. In pathological conditions, the demand for such energy increases significantly, and the body's own microvibration generation is impaired for a number of reasons. Fonovit affects the body with natural and crucial mechanical microvibrations, thus ensuring high effectiveness and safety in this therapeutic method.

For heel spurs, the Vitafon will help in most cases. It all depends on the number of treatments required to alleviate the pain and allow the tissue to regenerate. While we recommend having at least one Vitafon device at home, the results will depend on the time allocated for treatments, the size of the bony growth, and the degree of degradation of the plantar fascia.
NOTE
Before beginning any treatment, please consult with your doctor or physiotherapist to discuss your symptoms and receive a clear diagnosis.